What are haemorrhoids?


Haemorrhoidal disease is one of the most common human ailments. Maimonides4, an ancient physician from al-Andalus (1135-1204 AD), already pointed out the importance of diet and detailed a series of treatments to relieve the symptoms of haemorrhoids, including food broths, suppositories, creams or enemas to eliminate or prevent symptoms–they all non-surgical treatments.
Haemorrhoids (piles) are clusters of arteriovenous blood vessels forming a protrusion in the anal canal. When vascular tone is out of control and haemorrhoidal tissue degeneration occurs, normal anal cushions are symptomatically and abnormally shifted downward. Sliding anal cushions include abnormal dilation and distortion of the haemorrhoidal cluster, causing very uncomfortable and, in some cases, very severe symptoms.
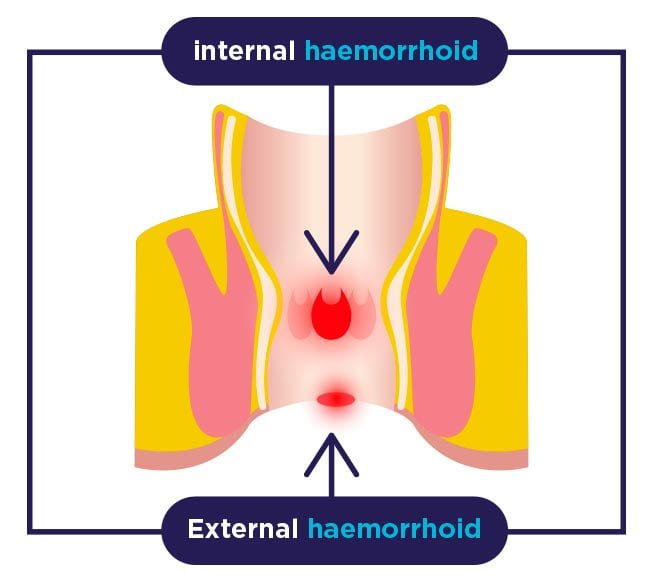
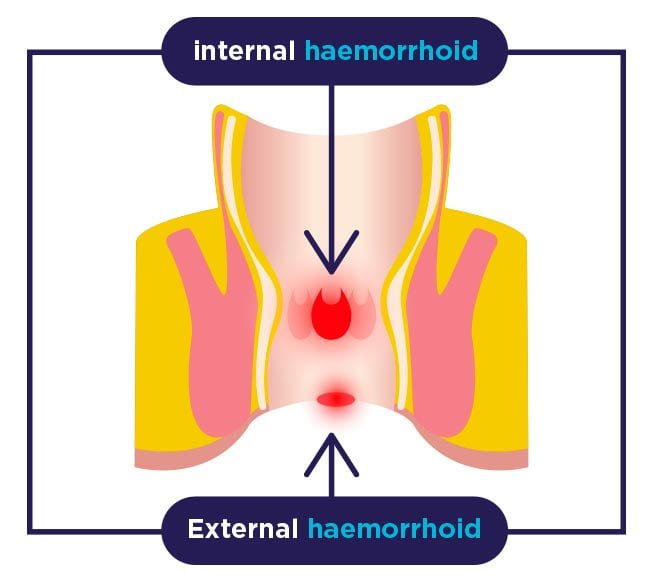
Haemorrhoids are generally classified depending on the location: internal (located in the rectum and covered by anal mucosa), external (with origin at the anal opening and covered by anoderm) and mixed.
The main symptoms of haemorrhoids include:
- Anal pain, especially while seated.
- Anal pruritus or itching.
- Blood on toilet paper, in faeces or in the toilet bowl.
- Pain during defecation.
- One or more hard and sensitive bumps near the anus.


One of the most common health problems among middle-aged adults
There are different causes that can trigger the occurrence of haemorrhoids, being constipation the most prevalent as there is greater effort during evacuation and therefore more pressure on the anal cushions. However, alcohol, spicy foods, diarrhoea, pregnancy, occupation and sedentary lifestyle, should be considered as predisposing factors. It is more frequently related to Western societies, possibly associated with low fibre consumption.


Treatments
Alternative or non-surgical treatments include: diet and changes in lifestyle, adding to diet hydrophilic agents such as Psyllium plantago seeds. Ointments or suppositories to treat haemorrhoidal disease are helpful. However, most of them only provide symptomatic treatment, but not a long-term solution. Other non-surgical options for haemorrhoidal disease comprise rubber band ligation, sclerotherapy, cryotherapy, bipolar coagulation, etc.


Cryotherapy
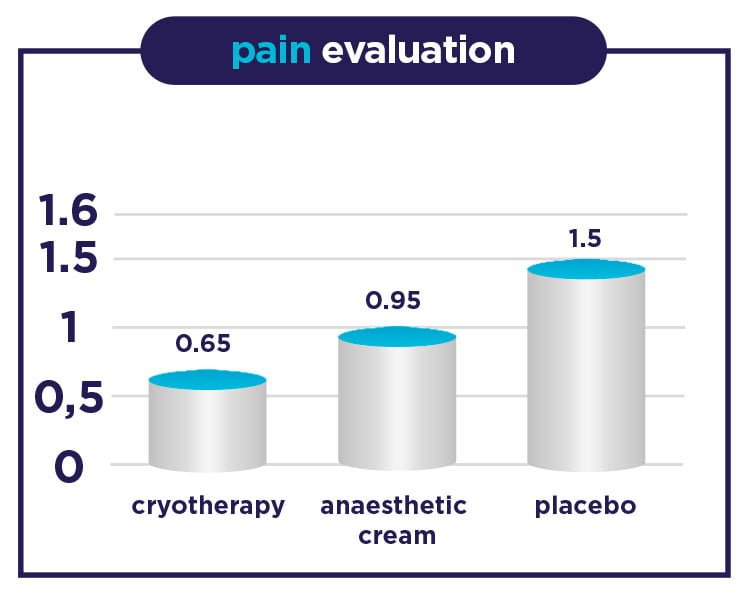
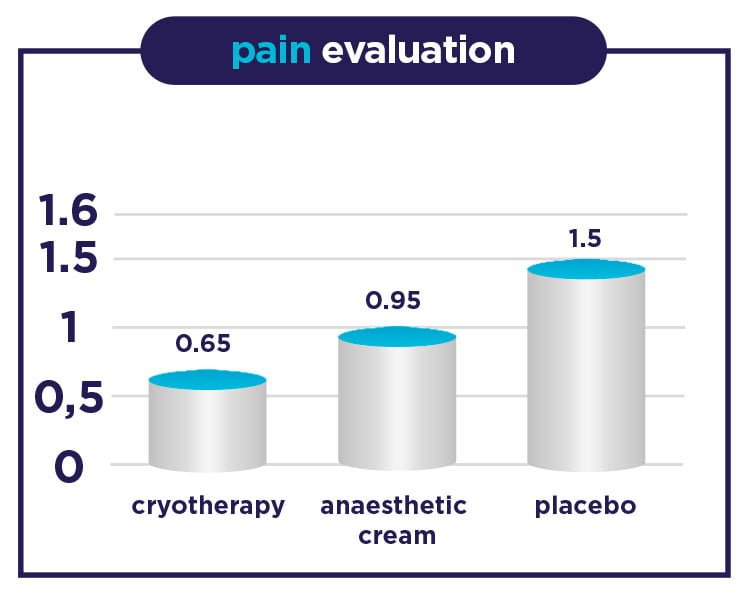
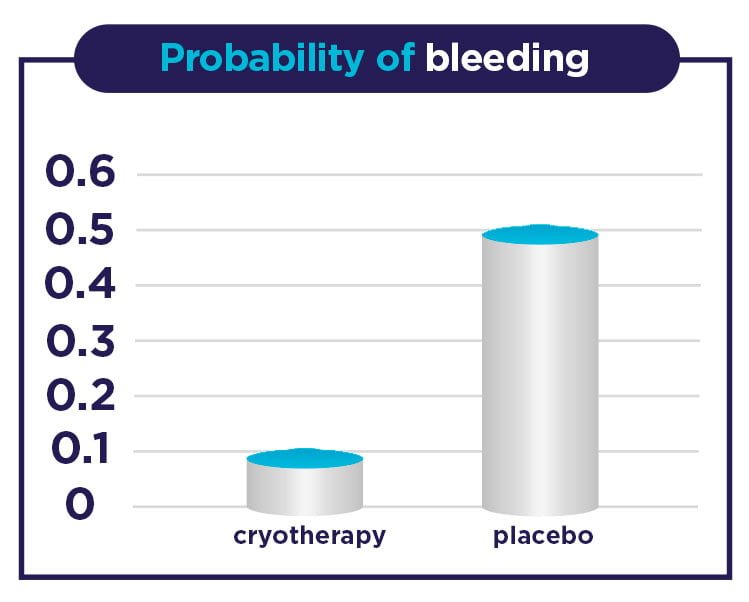
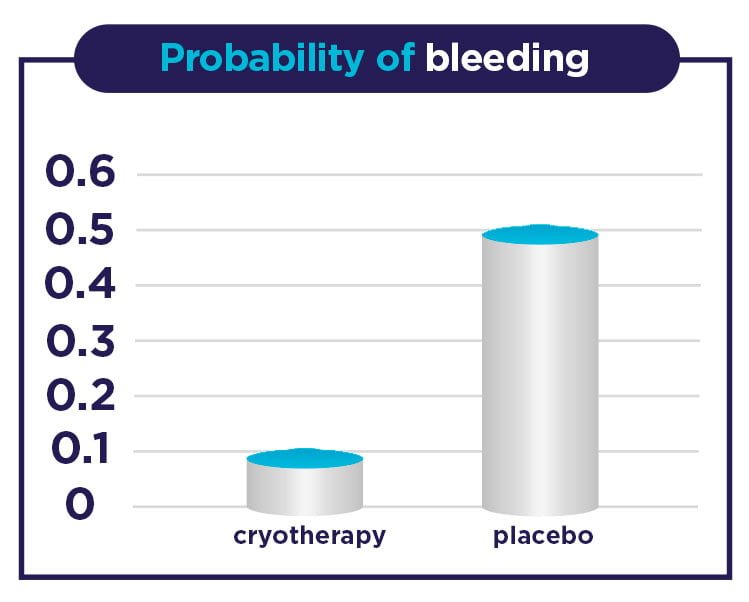
- There is pain reduction by more than 50% in individuals treated with cryotherapy vs. those not treated.
- Pain reduction by 20% in individuals treated with cryotherapy with regard to those treated with anaesthetic anti-haemorrhoidal cream.
It should also be highlighted that individuals in the cryotherapy device group showed no evidence of any kind of injury due to the design of the device or the temperature at which it is used, and pregnant women who participated showed no side effects.
1) Conte Vila, O. et al. Diciembre 2003. 2) Hemorrhoids and anal fissures. University of California, Berkeley. Appointments 510/642-2000. 3) Lohsiriwat, V. 2015 August 21. 4) Charúa Guindic, L. 2014.
